Direct experience with measles is rare for U.S. adults born after measles vaccination became available in 1963. Indeed, the disease was declared eliminated in this country in 2000. Unfortunately, it has had a resurgence in recent years and months, with a widely reported outbreak in West Texas that had spread to New Mexico and Oklahoma as of March 16. This outbreak has infected more than 290 people and been linked to two deaths. In the following Q&A, pediatric infectious disease expert Dr. Charles Prober answers basic questions about measles’ symptoms, effects, and transmission, and how it can be prevented.
Dr. Prober is a professor of pediatrics, immunology, and microbiology at the Stanford School of Medicine; senior associate provost for health education at Stanford University; and founding executive director of the Stanford Center for Health Education and its Digital Medic unit.
How dangerous is measles for children and for adults?
Prior to the availability of the first measles vaccine in 1963, this single virus was responsible for over 2.5 million deaths around the world each year. In the United States, 3 to 4 million cases of measles occurred each year, resulting in 400 to 500 deaths. Most of these deaths were in children less than 5 years of age and in the elderly. Deaths caused by measles usually result from infection of the lungs (pneumonia) and the brain (encephalitis).
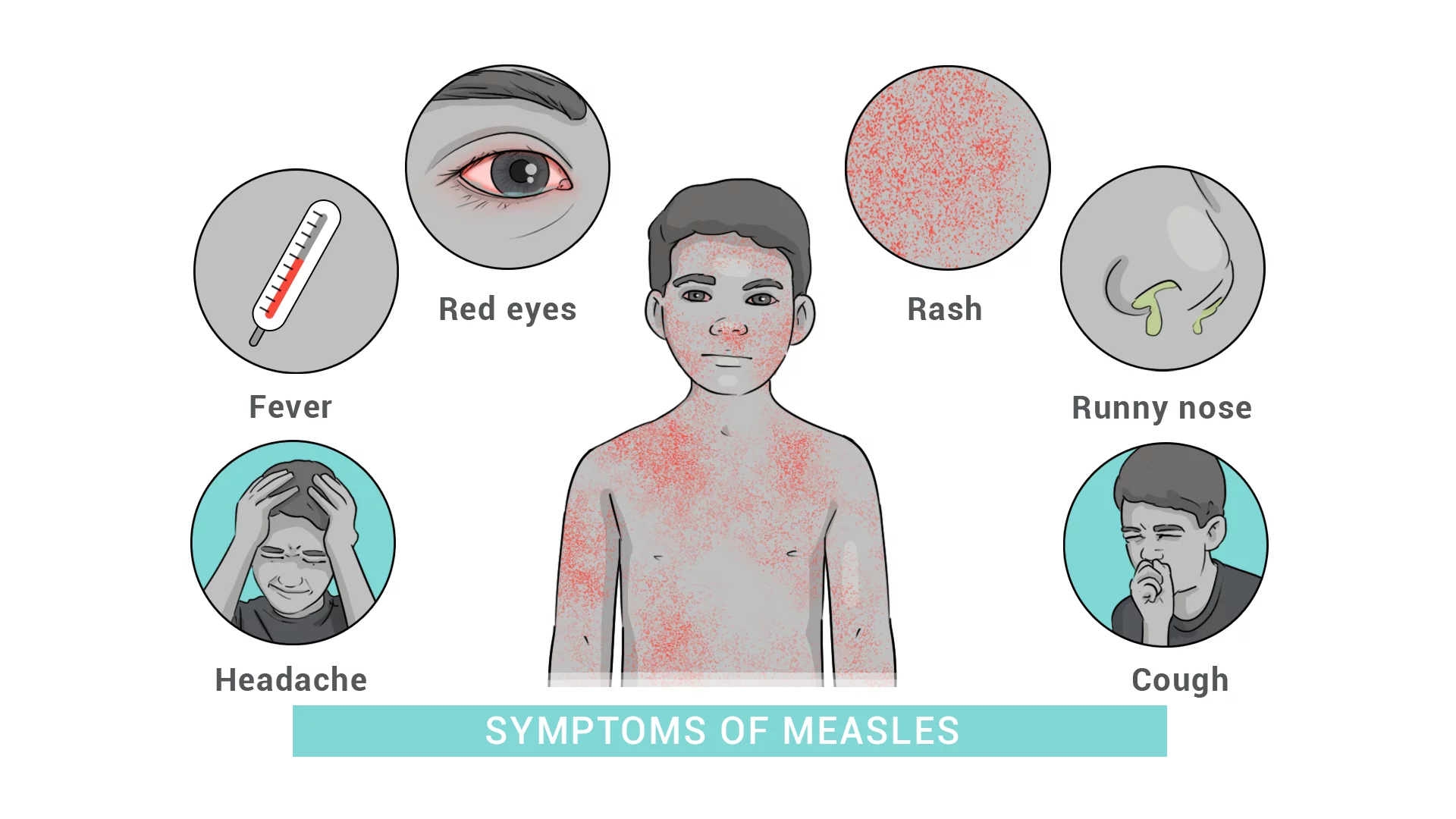
What are the symptoms of measles?
The first symptoms of measles, which start one to two weeks after exposure to another person who has the infection, include fever, runny nose, cough, and red eyes. This is followed by a red rash that typically starts on the face and rapidly spreads over the entire body. Fever and irritability increase as the rash spreads. Complications, including ear infections, pneumonia, and brain infection, occur about one to two weeks into the illness.
How contagious is measles?
Measles is the single most contagious infection throughout human history. In unvaccinated communities, a person with measles will infect 12 to 18 susceptible contacts. In comparison, a person with COVID will infect only 1 to 2 susceptible others. Therefore, measles is about 10 times more infectious than COVID.
How effective is the vaccine?
Measles vaccine is very effective. After a single dose, 93% of measles infections are prevented, and after two doses, 97% of infections are prevented. In the United States, the first dose is typically given between 12 and 15 months of age and the second between 4 and 6 years of age, just before kindergarten. This two-dose recommendation was introduced in 1989. Most people born prior to 1989 will have received only a single dose of measles vaccine.
It is important to note that because measles is so infectious, to protect an entire community, more than 95% of that community need to be vaccinated. This has been demonstrated in Texas, where an outbreak of over 250 cases of measles is ongoing due to a high population of unvaccinated children. One previously healthy child tragically died of this preventable infection, and an adult in New Mexico died after testing positive for measles.
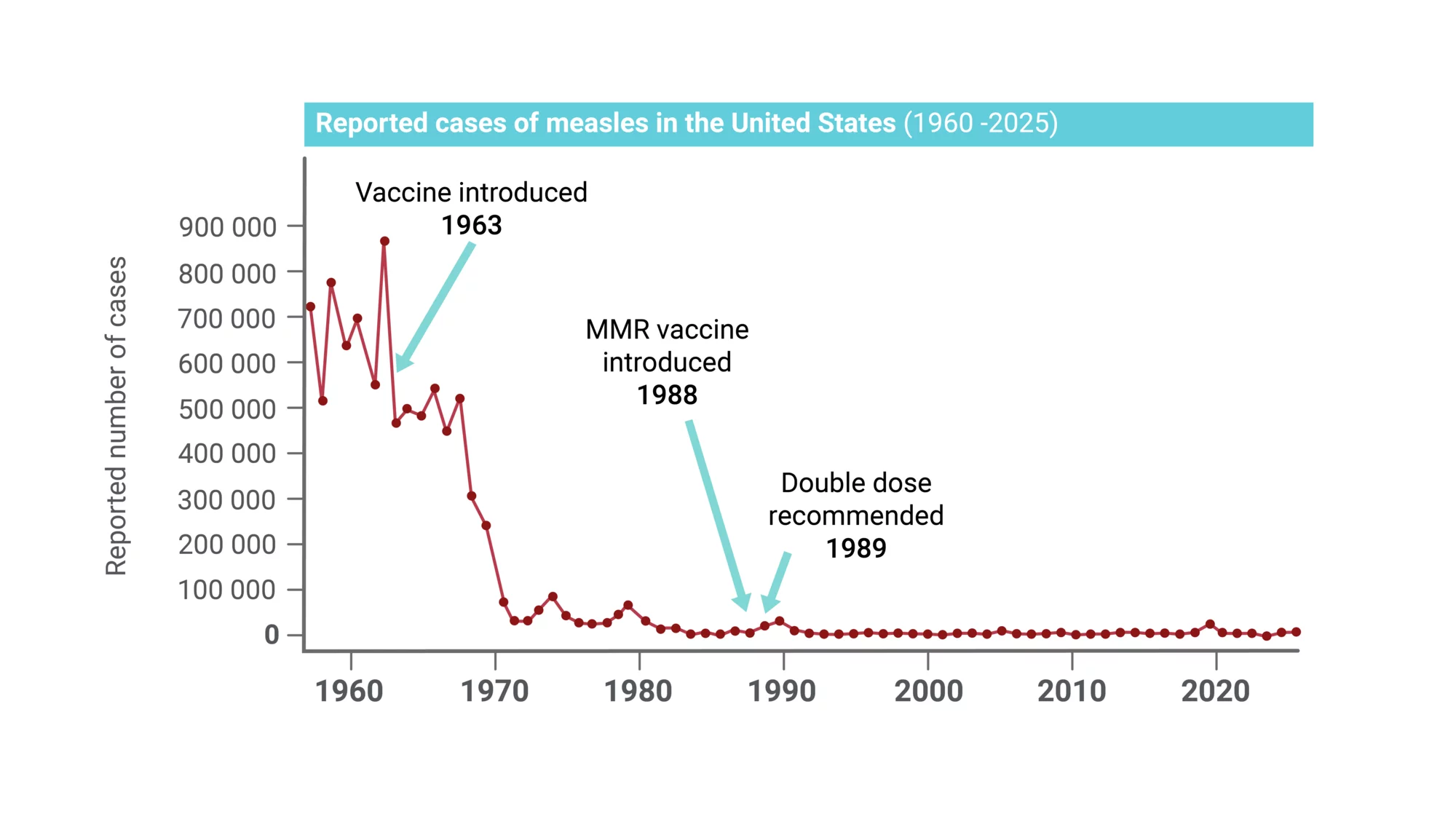
Measles cases in the US fell dramatically after the measles vaccine was introduced in 1963 and improved in 1968.
What are possible side effects of the vaccine?
Measles vaccine, whether given alone or in combination with mumps and rubella (MMR) or mumps, rubella, and varicella (MMRV), is well tolerated. The most common side effects include pain with possible redness and mild swelling at the injection site, and fever, sometimes with a mild rash about 2 weeks after the vaccine is given. Other rare side effects are described in my YouTube video, “Measles vaccines and infection prevention.”
What are your recommendations to parents whose children are not already vaccinated?
If your child has not been vaccinated, I strongly encourage you to arrange for vaccination as soon as possible. The current measles outbreak that began in Texas has spread to nearby states. It is painful to see a child suffer the serious complications that can accompany measles, sometimes leading to hospitalization and long-term consequences, including brain damage. Fortunately, death from measles in the United States is uncommon unless there is an underlying disease such as a weak immune system or cancer.
What should adults who have not been vaccinated, or who were vaccinated a long time ago, do?
Adults born before 1957 do not need to be vaccinated because most older adults had measles in their youth and enjoy lifelong protection. If you were born between 1957 and 1968 and you do not have a history of measles, you may be susceptible to measles. This is because the first measles vaccine was not in use until 1963, and it was not improved until 1968. If you were born after 1968, even if you only received a single dose of the measles vaccine, you are likely protected and do not need to be vaccinated again.
Under any of the above circumstances, your doctor may order a blood test to determine if you had a prior measles infection. If you have no evidence of a previous infection (no antibodies against measles in your blood), vaccination would be a good idea.
What impact does measles have worldwide?
According to the World Health Organization, deaths from measles had fallen to 107,500 globally in 2023, primarily in unvaccinated or undervaccinated children under age 5. That number speaks both to the success of vaccination initiatives (prior to the vaccine, measles caused an estimated 2.5 to 2.6 million deaths per year worldwide) and to the heartbreaking costs of their incomplete reach. At Digital Medic, we believe that accessible and accurate information is an essential building block for people everywhere to be able to address urgent health challenges and make informed decisions about their own health and that of their communities.
Watch to learn more about measles
Explore basic facts about measles: what it is, how it spreads, and common signs and symptoms.
Learn who is most at risk of complications and death from measles, and how it is diagnosed and treated. Supportive treatment is recommended as there is no antiviral therapy for measles and antibiotics are not effective against viral infections.
For more information
This interview was conducted via email by Jenny Robinson, interim communications lead at Digital Medic, Stanford Center for Health Education.
Digital Medic works to expand access to health information for health workers and community members worldwide. Join our email list to learn about new health education resources, breakthroughs in research, and opportunities to collaborate.
This story was originally published by Digital Medic, Stanford Center for Health Education.