Much remains unknown about how SARS-CoV-2, the virus that causes COVID-19, spreads through the environment. A major reason for this is that the behaviors and traits of viruses are highly variable – some spread more easily through water, others through air; some are wrapped in layers of fatty molecules that help them avoid their host’s immune system, while others are “naked.”
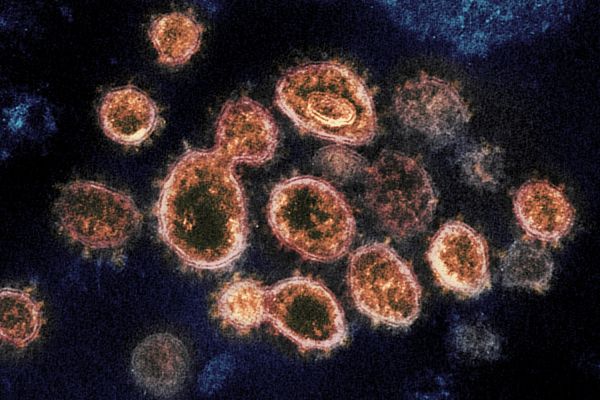
This transmission electron microscope image shows SARS-CoV-2, the virus that causes COVID-19. (Image credit: NIAID-RML / Flickr)
This makes it urgent for environmental engineers and scientists to collaborate on pinpointing viral and environmental characteristics that affect transmission via surfaces, the air and fecal matter, according to Alexandria Boehm, a Stanford professor of civil and environmental engineering, and Krista Wigginton, the Shimizu Visiting Professor in Stanford’s department of civil and environmental engineering and an associate professor at the University of Michigan.
Boehm and Wigginton co-authored a recently published viewpoint in Environmental Science & Technology calling for a broader, long-term and more quantitative approach to understanding viruses, such as SARS-CoV-2, that are spread through the environment. They are also principal investigators on a recently announced National Science Foundation-funded project to study the transfer of coronaviruses between skin and other materials, the effect of UV and sunlight on the coronaviruses, and the connection between disease outbreaks and virus concentrations in wastewater.
Below, Boehm and Wigginton discuss knowledge gaps, potential implications for safe water, promising research pathways and other issues related to the control of viruses such as SARS-CoV-2.
As environmental engineers, what do you think are some of the biggest gaps in our understanding of and ability to control viruses such as SARS-CoV-2?
Boehm: We don’t have a good understanding of what virus characteristics and environmental factors control virus persistence in the environment – for example, in aerosols and droplets, on surfaces including skin and in water including seawater. When a new virus emerges and poses a risk to human health, we don’t have a good way of predicting how it will behave in the environment.
Part of the problem is historically there has been limited funding for this sort of work. The National Institutes of Health historically hasn’t funded work on pathogens in the environment, and funding at the National Science Foundation for this work is limited. Also, coronaviruses and most of the emerging viruses that have caught the world’s attention over the last decade are enveloped viruses that are wrapped in an outer layer of fatty lipid molecules that they’ve stolen from their hosts. Proteins on the surface of the envelopes can help these viruses evade the immune systems of the organisms they are infecting. There has been much more work on the fate of non-enveloped or naked viruses because most intestinal pathogens in excrement are nonenveloped viruses – like norovirus and rotavirus.
Are viruses such as SARS-CoV-2 a threat to our water sources?
Boehm: We usually only worry about viruses in water if they are excreted by humans in their feces and urine. Most enveloped viruses aren’t excreted in feces or urine, so they aren’t usually on our minds when it comes to our water sources. There is increasing evidence that the SARS-CoV-2 viruses, or at least their genomes, are excreted in feces. If infective viruses are excreted, then fecal exposure could be a route of transmission. It’s unlikely this could be a major transmission route, but a person could potentially be exposed by interacting with water contaminated with untreated fecal matter.
Wigginton: We’ve designed our drinking water treatment systems with lots of treatment barriers to remove the most prevalent viruses and the most difficult-to-remove viruses. Research on viruses similar to the SARS-CoV-2 virus suggests they are susceptible to these treatments. In terms of virus concentration and persistence, this isn’t a worst-case scenario.
What are some promising or critical research areas for informing our response to viral outbreaks?
Boehm: If we could develop models to predict the environmental survival of novel viruses, that would be a huge step forward. To do so, we need to understand mechanistically how different characteristics of the virus such as size and composition affect how environmental factors – such as temperature and disinfectants – control their survival.
There are also opportunities to better understand how human behavior plays into viral transmission. For example, knowledge about how efficiently a virus can move from a surface to a hand should be informed by the kinds of surfaces that people actually touch, and can, in turn, inform health behavior interventions that will actually reduce exposure.
You write that “environmental science and engineering researchers should take a broader, long-term and more quantitative approach to understanding viruses that are spread through the environment.” Can you elaborate?
Wigginton: We tend to study viruses very intensely when there is an outbreak, but the results from one virus aren’t easy to extrapolate to other viruses that emerge five years later. If we took a broader approach to studying many kinds of viruses, we could better understand the characteristics driving their environmental fate.
Boehm: We need to make sure that observations about virus persistence in the environment are quantitative so they can be extended to understanding virus persistence in other contexts. Sometimes researchers present qualitative observations about viruses in the environment when they are not of immediate importance to their study. For example, some of the early reports of SARS-CoV-2 in feces were reported as numbers of gene copies of the virus per swab sample without reporting the mass of feces on the swab. Unfortunately, these data alone do not allow extrapolation to predict the concentrations of SARS-CoV-2 in wastewater or excrement, which many people would like to know from both a concern over risk, as well as an interest in using wastewater as an epidemiological tool.
How can experts from different disciplines collaborate research efforts to maximize their value to public health?
Wigginton: Environmental engineers and scientists are mostly looking at pathogens outside of the host. They are detecting pathogens in environmental samples, understanding their environmental fate or designing approaches, such as water disinfection, to remove them from the environment. Meanwhile, virologists are studying what happens within the host cells, and public health scientists are trying to understand people’s exposure to the virus and how it circulates through communities.
Research questions and techniques are sometimes quite similar across these fields. So, by working together we can move methods forward faster. Working across disciplines can lead to discoveries and strategies that wouldn’t be possible independently.
To read all stories about Stanford science, subscribe to the biweekly Stanford Science Digest.
Boehm is also a senior fellow at the Stanford Woods Institute for the Environment and an affiliate of the Stanford Program on Water, Health & Development.
Media Contacts
Rob Jordan, Stanford Woods Institute for the Environment, (650) 721-1881; rjordan@stanford.edu