Public health officials have a tough choice to make when it comes to screening people for HIV: administer a reliable blood test that can detect infections early on, but that few people will volunteer for, or give people a convenient test using saliva that is less reliable during the first stages of infection.
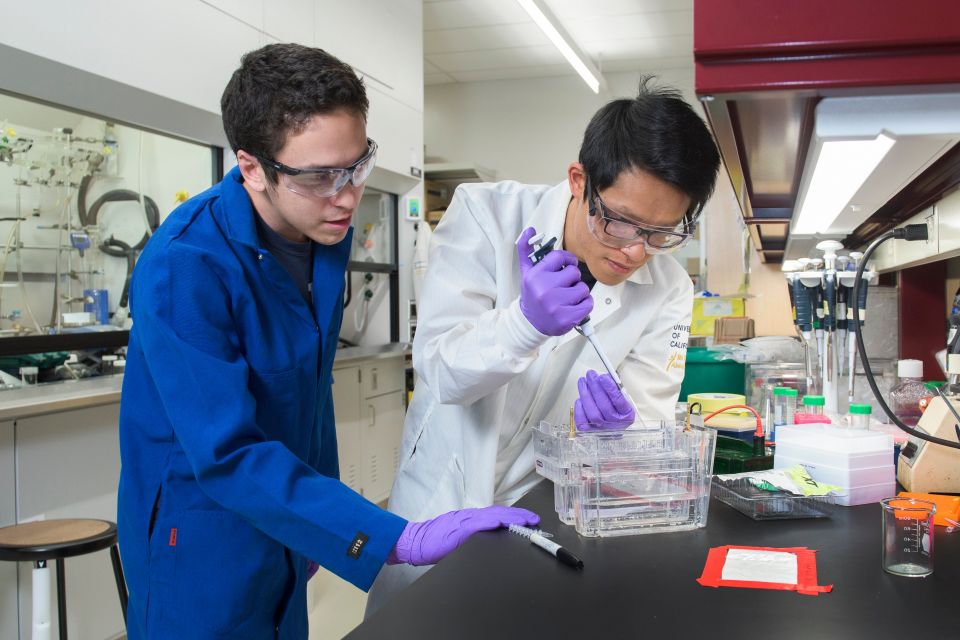
Cheng-ting “Jason” Tsai, a graduate student in the lab of Carolyn Bertozzi, and Peter Robinson, a former graduate student of Bertozzi’s, in 2016, work on an earlier version of their test. (Image credit: L.A. Cicero)
A new test could change that. Developed by Stanford chemists in collaboration with the Alameda County Public Health Laboratory, the test combines the convenience of spitting in a cup with the reliability of blood tests, they report in the January 22 edition of the Proceedings of the National Academy of Sciences.
“The earlier you can detect, the better, because people can infect other people,” said Carolyn Bertozzi, the Anne T. and Robert M. Bass Professor in the School of Humanities and Sciences and a professor of chemistry. “Every day that goes by that a person’s behavior is not modified based on their HIV status is a day that they could be infecting other people, especially for young people,” said Bertozzi, who is also a faculty fellow of Stanford ChEM-H and a member of Stanford Bio-X.
Brief history of HIV testing
By far the most common way to test for HIV infection is to look in a blood sample for antibodies, proteins that the immune system custom-builds to attack the virus and fight back against infection. That test is far more convenient than a direct search for the virus, in part because antibodies are relatively abundant in the bloodstream after the early stages of infection.
Professor Carolyn Bertozzi describes the new needle-free HIV test as “purposefully low tech.” (Image credit: L.A. Cicero)
Yet there is a major drawback, especially for public health officials and researchers who want – sometimes need – to get a lot of people tested quickly to help contain the spread of the disease: needles.
“There’s a lot of populations you just can’t reach out to by blood tests,” said Cheng-ting “Jason” Tsai, the lead author on the new paper and a graduate student in Bertozzi’s lab. “But if you were to do oral fluid, then all of sudden you open up a brand new population that was not otherwise accessible to you.”
But oral fluid tests have their own problems. While there are HIV antibodies in saliva, they do not accumulate at the levels they do in blood, or at the same speed – meaning that there just aren’t that many present, especially early on.
By the time oral fluid tests can reliably detect HIV, Bertozzi said, “you’ve waited a long time” – and in that time, the infection could spread.
Translating HIV
The team’s job, then, was to figure out how to make it easier to detect the small amount of antibodies present in the saliva of someone with HIV. To do that, they took an indirect approach. Instead of looking for the antibodies themselves, they looked for what antibodies could do.
The team took advantage of a key feature of antibodies – they have two arms, each of which easily latches onto a virus like HIV. They took bits of HIV and attached them to one or the other half of a piece of DNA. They then added the modified HIV bits into the saliva sample. If the sample contained HIV antibodies, their two arms would grab hold of the tagged HIV, bringing the two halves of the DNA together into a continuous strand. Once the DNA piece is made whole it is easy to detect using standard lab techniques.
That can all be done without requiring a blood sample or much technology to process the samples that are taken. “It’s purposefully low tech,” Bertozzi said.
Although the researchers say it will take more studies to confirm the results, the first experiments show that it works well: the test correctly diagnosed 22 people who took part in an Alameda County screening effort, each of whom had tested positive for HIV using other methods. Importantly the test did not falsely detect HIV in the 22 additional HIV-negative participants.
It may also work earlier compared to other saliva tests, although not earlier than existing blood tests. In a set of eight samples that had produced mixed results with the current standard saliva test, six turned up positive with the new HIV test, and one of those was confirmed using a blood test. Although those results are preliminary, they suggest that the new test is more sensitive and could pick up HIV infection sooner than others.
“Our hope is that we can get an earlier read than the present oral test because the sensitivity is better,” Bertozzi said. Beyond HIV, she and Tsai said, the same principles may be useful for allergy testing and screening for typhoid and tuberculosis infection. The team is also investigating the method as a way to test the efficacy of measles vaccination efforts, Bertozzi said.
Bertozzi is also a member of the Child Health Research Institute, the Stanford Cancer Institute and the Stanford Neurosciences Institute. The research was supported by grants from the Stanford Predictive and Diagnostics Accelerator, the National Science Foundation and the National Institutes of Health.
Media Contacts
Nathan Collins, Stanford News Service: (650) 725-9364, nac@stanford.edu