Stanford course explores the principles, applications, and implications of medical imaging
An introductory seminar dives into the technologies behind the shadowy photos of anatomy that give clinicians a window into our most personal of spaces.
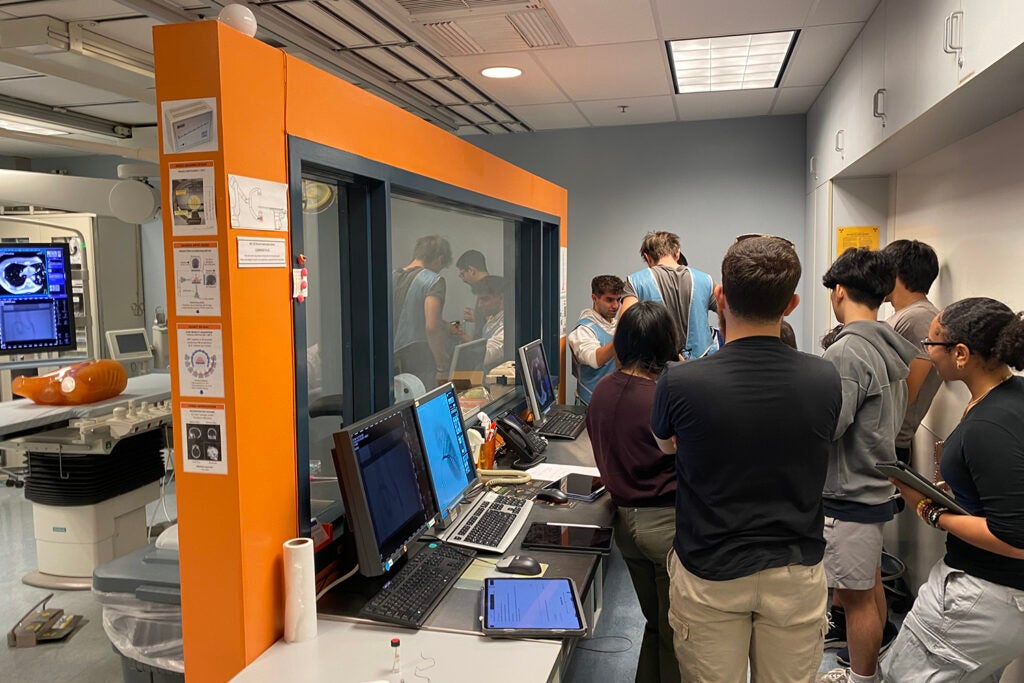
Students at the operating console of radiology Assistant Professor Adam Wang’s X-ray lab. On the other side of a radiation-blocking lead wall is the robotic scanner that performs the X-ray. (Image credit: Daniel Ennis)
In the Richard M. Lucas Center for Imaging on Stanford’s medical campus, radiology Professor Daniel Ennis and Instructor Marios Georgiadis stand in a dispersed circle of students, all eyes on a key that the two men pass between them. At the center of the room, one of approximately 30 PET/MRI (positron emission tomography/magnetic resonance imaging) machines in the United States hums with electricity. Its hulking white frame conceals a superpowered magnet. The instructors carefully share the key with the students, urging them to approach the mouth of the machine and experience the pull of attraction.
These students are Stanford frosh and sophomores in the introductory seminar course The Magic of Medical Imaging (RAD 21Q) and this is the practical lab component of a unit on PET. This is a type of imaging that tracks metabolic changes in organs and tissues with small amounts of radioactive tracer administered intravenously. It’s commonly used to spot the spread of cancer.
Altogether, the course focused on PET and three other imaging technologies: ultrasound, which uses soundwaves and is most commonly used to monitor babies in utero; MRI, which creates visualizations through applying a strong magnetic field and radio waves and is especially useful for examining soft tissues and the nervous system; and computed tomography (CT), which uses X-rays to produce images of the skeleton, blood vessels, and other tissues.
To explore each of the four technologies, Ennis and Georgiadis cover the basic principles, applications, and implications. Students present new imaging research and discuss the financial burden, environmental cost, and health risks associated with each type of imaging.
“We’re both in the Department of Radiology, right?” said Ennis. “But neither of us has a radiology degree.” Radiology is not offered as an undergraduate degree at Stanford or anywhere and, in general, students don’t usually encounter the field until they’re in a specialty that uses the technology, like bioengineering. “That was part of the motivation for offering this class, there aren’t a lot of classes like this available to undergrads.”
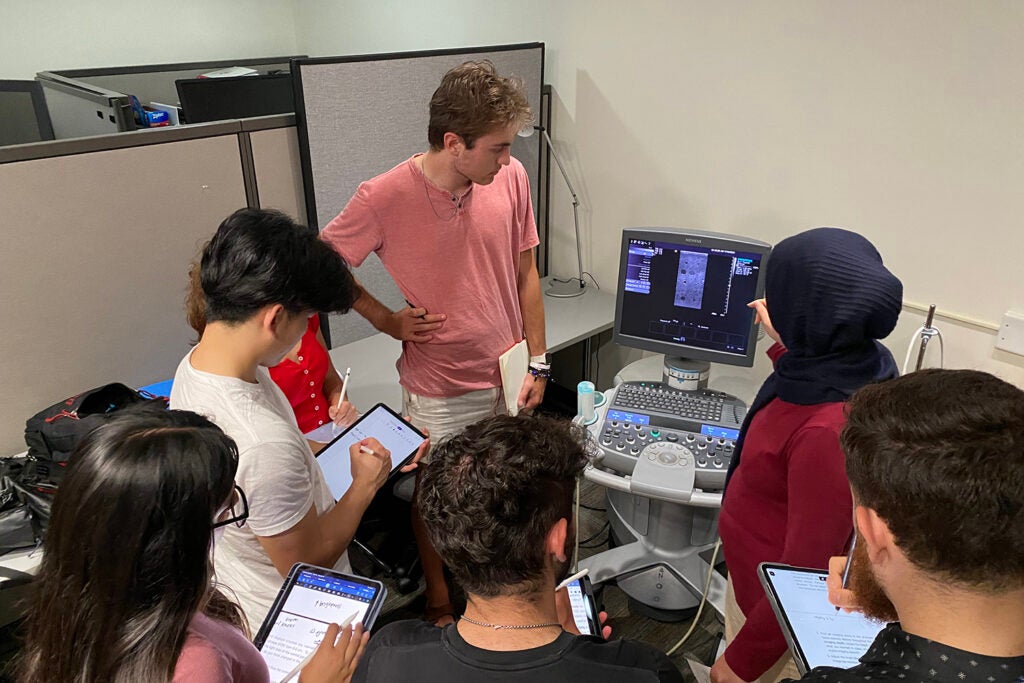
As part of the ultrasound lab, students were shown the effect of depth and object geometry on the ultrasound signal using a medical ultrasound probe on a training “phantom,” a synthetic model that mimics real tissue. (Image credit: Daniel Ennis)
The vision
Introducing undergraduate students to the work they love was one of the driving forces behind this course. Georgiadis approached Ennis about working together after Stanford radiology professor Kim Butts Pauly suggested radiology as an introductory seminar topic in a faculty meeting.
“We had never taught an IntroSem before,” said Georgiadis. “A year ago, we didn’t even know there were IntroSems.” Georgiadis, who works primarily with graduate and medical students, was excited about teaching students at the beginning of their academic careers. Ennis shared his enthusiasm, evidenced by the fact that the duo met every other week for close to a year to map out the curriculum. “We talked about intersectionality; the medical imaging topics – PET MRI, ultrasound, X-ray – and then their intersections with these other social world components,” said Ennis.
The instructors wanted the students to understand how these remarkable tools give radiologists a window into our most personal of spaces and learn about their routine and cutting-edge applications, but also realize the implications for patients and society when it comes to cost, environmental impact, accessibility, and safety.
Ennis and Georgiadis arrived at radiology careers from different directions. Ennis studied biomedical engineering, developed an interest in the heart, and then a passion for imaging it. He now runs the Cardiac MRI Research Group (CMRG) at Stanford. Georgiadis studied bone biomechanics as a mechanical and biomedical engineer, was fascinated by imaging technology and the intricacies of the brain and pivoted to neuroimaging. He is in the Translational Neuroimaging lab at Stanford.
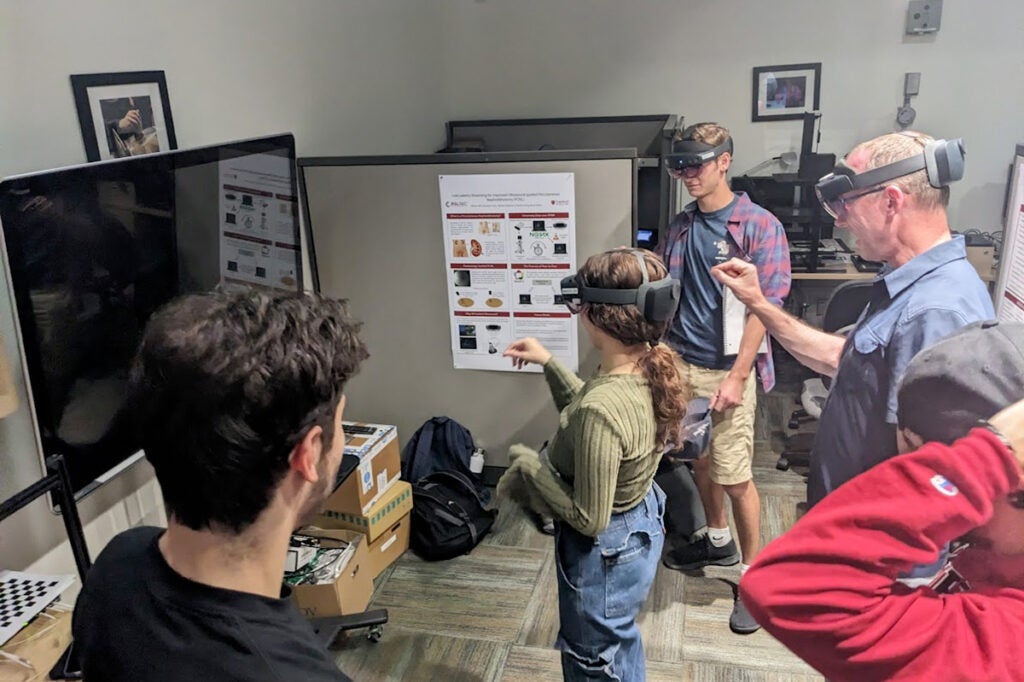
In a module on augmented reality, students experienced how people can train virtually for medical tool handling and interact with virtual objects and anatomy. This was a portion of their ultrasound lessons and took place at the Incubator for Medical Mixed and Extended Reality at Stanford. (Image credit: Marios Georgiadis)
Personal insights
The course was designed for any student who shares a fascination with the secret world within. For some, it’s an introduction to the medical field, well-suited to students who are interested in pursuing a career in medicine. For others, it’s an invitation to think deeply about the technology we intersect with as patients. For many, a personal experience with medical imaging inspired them to enroll.
“I had a heart transplant in the spring, and I was exposed to most of the imaging modalities,” said sophomore Andreas Cannon Lorgen, a computer science major. The class on MRI was a highlight for him. “Dr. Ennis was talking about mainly cardiac MRI,” he said, “He talked a lot about the heart and heart function, and it was like oh, yeah, the reason I took this class is to be here right now.”
Lorgen’s experience with major surgery piqued his interest in medical imaging, but as the quarter progressed, he noticed a surprising amount of overlap with his computer science classes. “Even though this class is medically focused, a lot of it is about how the technology works,” he said. “There is definitely a scenario where I would work with this kind of technology or work in the medical field from a tech perspective.”
“I didn’t realize how complicated it was, how informative it can be – its power,” said first-year student Alice Finkelstein, who plans to major in bioengineering and go on to medical school after graduating. “Familiarizing myself with anatomy and the devices and technology available has been really useful, it’s a direct way for me to connect with my interests and definitely solidified my passion for this.”
As is often the case with the intimate connections formed in IntroSem courses, the journey for this cohort doesn’t necessarily end when the quarter does.
“You really get a personal relationship with the faculty,” said Lorgen, whom Ennis has offered to connect with colleagues in the cardiology department to talk about his personal circumstances. “You can always come back to them later, even after the quarter is over for feedback, advice, or mentorship. It’s a very unique opportunity.”
Ennis is also a member of Stanford Bio-X, the Cardiovascular Institute, and the Maternal & Child Health Research Institute (MCHRI).